Ultrasonic pelvimetry method for obstetricians
At first
Usually , pelvimetry is performed by X-ray or MRI. However, I insistent that pelvimetry can be done approximately even by ultrasonic tomography. As shown in Figure-1 , the longitudinal ultrasonic tomographic image of the pregnant pelvis provides information that approximates the Guthmann X-ray imaging method. But, the biggest drawback of my ultrasound method is that there is no information based on the transverse tomographic image of the pelvis. Ultrasound examiner can only obtain approximate information only for the longitudinal tomographic scanning at the pelvic inlet, but I still think that it is not useless information at all. I hope that it will be useful for daily medical care as a measure to avoid difficult birth.
(※ This method is almost powerless about diagnosis of CPD during labor. As before, I would like you to perform pelvic measurement by X-ray or MRI.
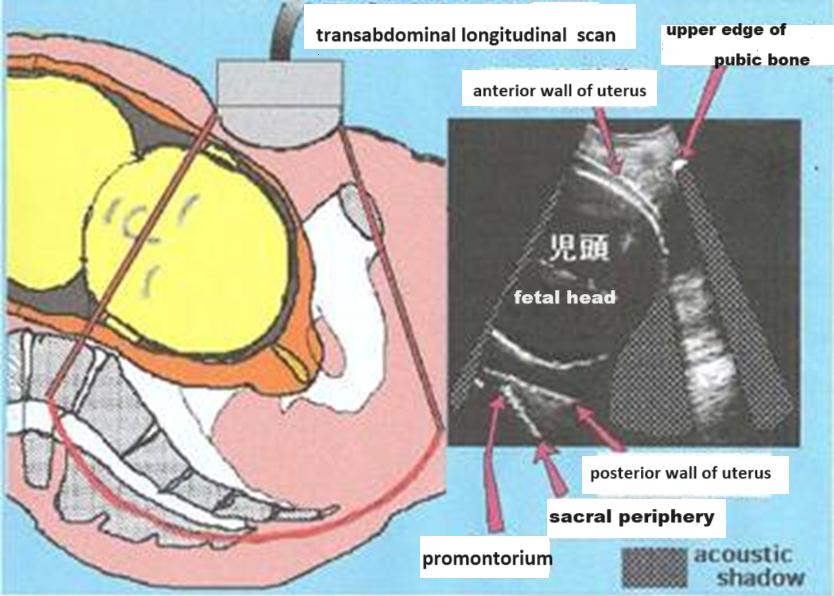 Figure-1
Figure-1
As shown in Figure 1, you can view a profile image of the inlet of the pelvis with a convex scan. Note that acoustic shadow occurs as shown in the figure, but there is a place below the baby's head where no shading occurs, and the sacral periphery image can be detected. The top and bottom of the baby's head create acoustic shadow, but most parts of the baby's head are highly permeable to ultrasound and act as just as "windows" acoustically. I think that the baby’s head is “acoustic window”.
It is possible to examine the anteroposterior diameter of about 4~5 cm in depth from the entrance of the tunnel called the pelvis by ultrasound . OC (obstetric conjugate) and PA (pelvic aperture angle; pelvic opening angle) can be known approximately by ultrasonic tomography.
The useful point of ultrasonic testing is that it can be inspected again and again. From about 28 weeks of pregnancy, it can correct the misunderstandings and unavoidable errors in the ultrasonic examination by repeating examination each prenatal checkup.
Since the degree of descent into the pelvis of the advanced fetal head can also be known, it can be applied to the management of premature birth in addition to prevention of difficult birth. This time, I will publish some parts of the ultrasound diagnostic method that I have done.
1.Measurement method of UOC (ultrasonic obstetric conjugate)
The UOC was proposed by Kagoshima University Obstetrics and Gynecology in 1998. →Reference. 1)
OC (obstetric conjugate) should originally be measured by X-ray pelvimetry.
TThe reason will be described later, but it seems impossible to accurately measure OC like X-ray by ultrasound. However, by devising the scanning method a little, it is possible to get the measurement value which approximates OC measured by X-ray. You can obtain the ultrasonic image which is very similar to The Guthman X-ray photography. “Although it’s not exactly right, it’s not far off.” The UOC is not exactly OC, but it is close to the OC.
1. Ultrasonic images of the pubic bone and symphysis
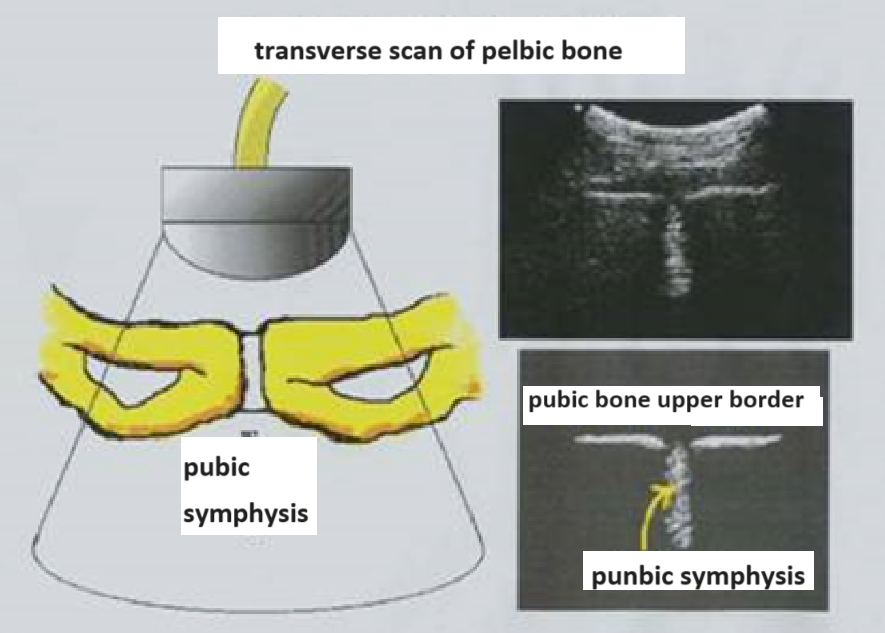 Figure-2
Figure-2To understand the descriptiveness of the pubic bone and symphysis, try the transverse scan first on the pubic bone as shown in the Figure-2.
In that case, it is necessary to apply enough jelly to the probe because the pubic hair interferes with reading.
The pubic symphysis is depicted as an echo image like the elephant’s trunk that extends long below.
Since the pubic symphysis is not bone tissue, ultrasonic attenuation is small, and it is drawn to the depths. the upper border of pubic bone on both sides is depicted as a high-intensity line image like a bird's wing.
If you understand this transverse image of the pubic bone and symphysis can be applied to the diagnosis of postpartum pubic symphysis separation. The Figure-3,4 is an ultrasound transverse image of the pubic bone of the case in which the pubic symphysis was separated.
 Figure-3
Figure-3 Figure-4
Figure-4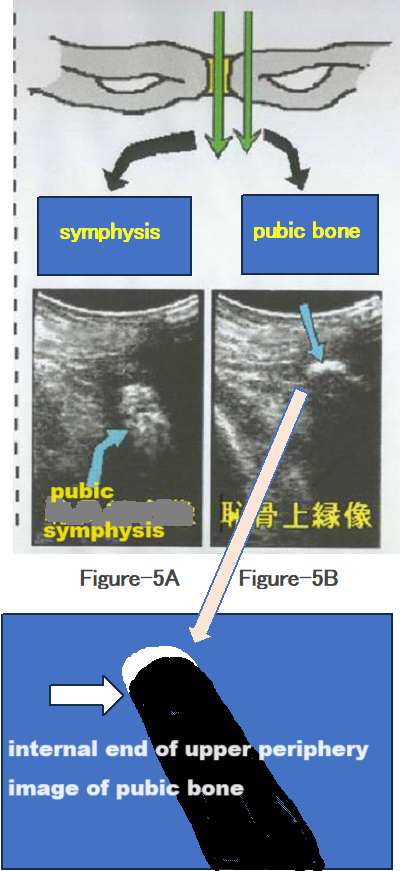 Figure-5A / Figure-5B
Figure-5A / Figure-5BNext, when the longitudinal scan is done on pubic bone, the pubic symphysis is depicted as an oval and slender image of the middle brightness as shown in Figure-5A, but this image seems not to be able to be clearly observed in all cases during pregnancy.
Moreover, the boundary is ambiguous because the inside of this oval image becomes the far opposite side (back side) in the ultrasonic incident direction, and it seems to be inappropriate for the UOC to be start point of measurement.
When a longitudinal scan is performed on the pubic bone close to symphysis, the superior periphery of pubic bone (very bright crescent-shaped image) is depicted as shown in Fig. 5B, and acoustic shadow occurs below it. This image of pubic bone is clearly depicted in all cases. The internal end of this very bright crescent-shaped image is the source of the starting point for measuring UOC.
2. Posterior uterine wall image, sacral periphery image and promontory
Please try to do the pelvic longitudinal scan of the postpartum woman because it is good experience to become familiar with the reading of the sacral periphery image and promontory.
Figures 6 and 7 show pelvic longitudinal scan images of postpartum women on the second day after childbirth. Since the postpartum uterus occupies most of the pelvis, the sacral periphery under uterus can be clearly read as a high-intensity line image. I think that it is possible to understand the posterior uterine wall image and the sacral periphery image clearly by this experience.
The post-uterine wall is compressed at the promontory, and I think that it is understood well that the sacral periphery image and the post-uterine wall image are close near the promontory.
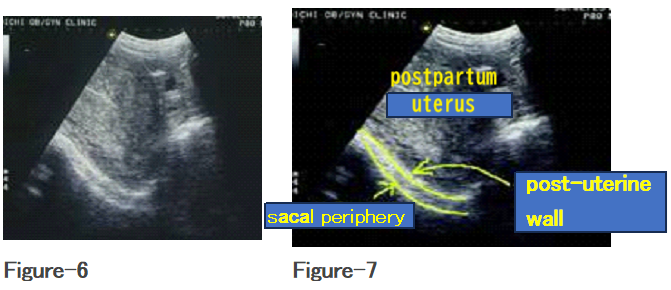
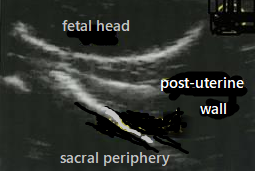 Figure-8
Figure-8Figure-8 shows an enlarged image near the promontory of a pregnant woman at 36 weeks of pregnancy. The post-uterine wall and the sacral periphery are drawn as similar high-intensity line images.
Therefore, it is necessary to be careful because the post-uterine wall image may be mistaken as a sacral periphery image. In fact, sometimes this can be difficult to identify, and this is the problem with UOC measurements.
3. Disturbing factors for imaging of sacrum
A) Acoustic shadow at the top and the bottom of the fetal skull.
The central part of the baby's head has less ultrasonic attenuation and the ultrasound passes through without attenuation, so it serves as an acoustic "window", and it can help to read the sacral periphery, but acoustic shadow occurs at the top of the fetal skull and below the bottom of the fetal skull, so it becomes obstacles in the sacral reading.
In the case of a floating baby head, the acoustic shadow of the top of the fetal skull hides near the promontory, so it will be difficult to read the sacral periphery.
B) Sometimes, the sacral periphery may not be obvious due to a stool mass in the rectum.
C) Ultrasonic multiplex reflexes may occur between the fetal skull and the uterine wall, and the sacral periphery may not be detectable.
4. Longitudinal scanning method at the inlet of the pelvis
Initially, we tried to measure OC by carrying out a longitudinal scanning on the middle line connecting the pubic symphysis and the promontory, but this did not work well.
As mentioned above, the pubic symphysis image (Figure-5A) is not clearly detected in all cases, so it is often not possible to set an accurate measurement start point on the pubic bone side. In addition, the measurement start point of OC is inside of the symphysis, but it is impossible to identify this point by ultrasonic tomography because the inside of the symphysis is on the far opposite side (back side) in the ultrasonic incident direction.
This is the basis for the decision that it is impossible to measure the OC by ultrasound. If I gave up my research here, it would be impossible to measure my pelvis by ultrasound forever, so I had to change my way of thinking a little.
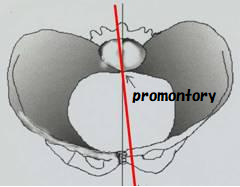 Figure-9
Figure-9Therefore, as shown in Fig. 9, we performed a longitudinal scanning a little diagonally toward the promontory from the pubic bone close to the symphysis, and we determined to measure the distance to the promontory using the superior periphery of pubic bone image (Figure-5B) as the starting point for measuring.
If measured in this way, the OC itself cannot be measured, but values close to the OC should be able to be measured. We decided to name it UOC (Ultrasonic Obstetric Conjugate) in consultation with Dr. Yoshinaga of Kagoshima University Obstetrics and Gynecology.
As shown in the Figures 10 and 11, the UOC will be measured slightly off the original obstetric true binding line (OC), and the UOC will always be measured 0.5 to 1 cm longer than the OC.
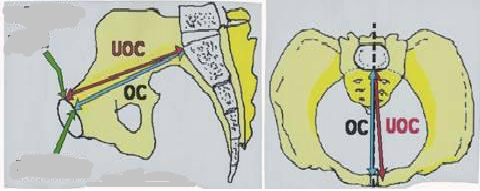 Figure-10/11
Figure-10/115. Measurement method of UOC (ultrasonic obstetric conjugate)
Let me explain in detail how to measure UOC. First, apply enough jelly to the convex probe, apply the probe to either the left or right pubic bone near the symphysis, and look for the superior periphery image of pubic bone (①in the Fig.-12). This image of pubic bone is fixed to the upper right corner of the ultrasound images, and the probe is moved using it as a fulcrum to find the promontory and sacral periphery image (③ and ④ in the Fig.-12).
Or, on the contrary, you may first look for the promontory and sacral periphery image, fix it in the lower left corner of the image, move the probe using it as a fulcrum, and look for the superior periphery image of the pubic bone.
A probe operation technique is required to draw the superior periphery of pubic bone in the upper right corner of the ultrasonic images, while at the same time drawing the sacral periphery and promontory in the lower left corner.
As shown in the figure below, the distance from the internal end of superior periphery image of pubic bone (bright part of a few mm width) to the promontory is measured as UOC.
When the fetal head is floating, acoustic shadow by the top of the head may make it difficult to identify the sacral image, and only the sacral image near the promontory may be drawn.
It seems that it is easier to confirm the sacral image if the fetal head has invaded the pelvis appropriately. However, when the baby's head descends too much, acoustic shading of the bottom of the fetal skull make it difficult to identify the promontory.
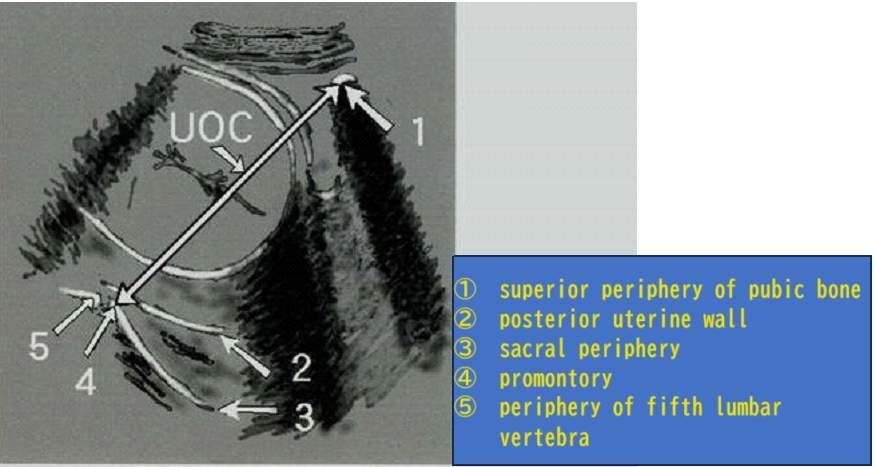 Figure-12
Figure-126. Evaluation of measurement values of UOC (ultrasonic obstetric conjugate)
The average value of UOC (ultrasonic obstetric conjugate) was 12.9 cm to 13 cm in a survey by Kagoshima University Obstetrics and Gynecology, and I think that the average value of UOC may be about 13 cm.
As for the average value of OC (obstetric true bond line), currently, "The average value of OC in modern Japanese women may be about 12 cm. There is an opinion that says.
In this way, there is a difference of about 1 cm in the average value of UOC and OC. The reason is due to the difference in the method of measuring ultrasound and X-rays, as mentioned above.
According to the definition of the Japanese Society of Obstetrics and Gynecology, the average value of OC (obstetric conjugate) is 11.5 cm, but this is too small and not very modern female, so I have a requirement to change this definition.
There are pregnant women who are 14 to 15 cm in large UOC. The average value of UOC in Westerners is probably larger.
In pregnant women with small UOC, of course, difficult births increase. Kagoshima University has found that pregnant women with UOC of less than 12 cm have an increase in the rate of cesarean sections and an increase in the incidence of fetal and neonatal asphyxia due to an increase in the tendency to have difficulties and prolonged delivery.
However, even if it is less than 12 cm, it may be surprisingly easy to give birth, but in such pregnant women, it seems that the pelvic aperture angle described later is often 90 degrees or more.
The figure below (Figure 13) shows a case with a UOC of less than 12 cm.
 Figure-13
Figure-137. Measurement of the UAPD (ultrasonic shortest antero-posterior diameter of the pelvic inlet)
Usually, the obstetric conjugate is the shortest antero-posterior diameter at the pelvic inlet, but in 10 to 20% of pregnant women, there may be a shorter diameter below the obstetric conjugate line.
As shown in the figure below, when the distance to the pubic bone is measured from the measurement point on the sacral periphery image about 3 cm below the promontory, it has been understood that there are not a few pregnant women shorter than UOC. It has been found that such pregnant women are easy to cause labor abnormalities.
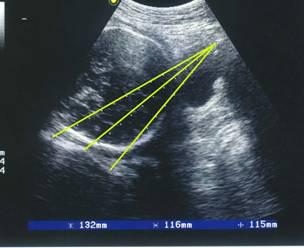 Figure-14
Figure-14 Figure-15
Figure-15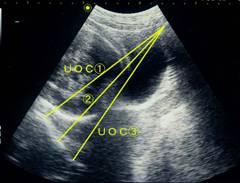 Figure-16
Figure-16Currently, pregnant woman in all cases, and as shown in the Figure 16, I measure the antero-posterior diameters of 2 to 3 places at the pelvic inlet.
As shown in Fig. 16, if you record it as UOC ①, UOC ②, UOC ③, etc., it is useful for diagnosing pelvic aperture angle and sacral morphological abnormalities described later.
The shortest of these UOCs is the shortest pelvic inlet antero-posterior diameter (UAPD) due to ultrasonic faults, and we are currently investigating whether it will be useful for diagnosing CPD. We have not yet reached a conclusion, but if the difference between the fetal BPD (UAPD-BPD) is less than 3 cm, the possibility of cephalopelvic disproportion (CPD) increases, and if it is less than 2.5 cm, I think that it may be diagnosed as CPD under ultrasonic tomography.
Even if UOC or UAPD is 12 cm or less, or UAPD-BPD is 3 cm or less, if the fetal head is sufficiently sinking and fixed in the pelvis, it is possible to somehow transvaginal delivery, but there is a high possibility of rotational abnormality and labor prolongation.
8. Measurement of PA (pelvic aperture angle)
Proposal of UPA (ultrasonic pelvic aperture angle)
The angle between the obstetric conjugate and the anterior periphery of the first sacral vertebrae is the pelvic aperture angle, but it is usually measured by Guthman X-ray imaging method. It is possible to measure this by ultrasonic tomography. With modern devices, it is also possible to measure the angle.
Dr. Hiromitsu Yamazaki, who has opened an obstetrics and gynecologist's office in Nagasaki Prefecture, strongly insists on the importance of PA. According to Dr. Yamazaki, the average PA is 86.6 degrees (X-ray data), and the smaller the PA, the more exponentially the probability of cesarean section increases. When managing labor, it is very important to predict difficult births, especially in the final stages of labor, but surprisingly there seems to be a situation where it is not used very clinically. I couldn't find an appropriate English translation of the PA, so in the opinion of Dr. Yamazaki, it was translated as “Pelvic aperture angle.”
The angle between the line connecting the point on the sacral periphery (about 3 cm below from the promontory) to the promontory and the UOC is measured as UPA (ultrasonic pelvic aperture angle).
In our study, the average UPA is about 88 degrees.
A survey conducted by Kagoshima University has found that if the pelvic angle is less than 80 degrees and the UAPD-BPD is less than 3 cm, the C/S rate significantly increases. UPA less than 80 degrees + UAPD-BPD 3 cm is easy to cause delivery stop, and it is necessary to closely monitor it because it may cause fetal asphyxia in stage II of labor.
In fact, I tried to submit this survey to the Japanese Society of Obstetrics and Gynecology in 1999 or 2000 (I don’t remember it very well anymore.), but unfortunately it was not adopted. Therefore, it is not something that can be said with much confidence. UPA is totally my personal advocacy. As I will talk about later, the ambiguity of the measurement method is a problem for UPA, and I think that is the cause of the failure of the Japanese Society of O & G.
9. Epilogue
I have been measuring UPA since then, but I think it will be impossible to show sufficient evidence because the measurement error is too large. When the angle is measured by the convex scan, the measurement value changes greatly with a slight change in the ultrasonic incident direction. However, if the measurement result with a pelvic opening angle of less than 80 degrees is produced many times, I have the impression that there are many cases where the birth becomes difficult.
"Pregnant woman's pelvis" seems to have the possibility of subtly changing its size and shape during pregnancy and labor. The tendency seems to become remarkable when the baby head of the fetus descends into the pelvis. At that time, the UOC and UAPD and UPA seems to fluctuate.
On the other hand, in the case of a floating baby head, the pelvis may appear to close its entrance tightly, as if rejecting the baby's head.
It cannot be denied that the measurement value of ultrasonic pelvimetry also has some measurement error, and it is a considerably ambiguous examination.
And it is thought that the size and shape of the pelvis itself change with the pregnancy progress, and for example, as the pelvis of the pregnant woman who initially judged it to be a very narrow pelvis descends, it seems that it may gradually spread when measured as 8 months, 9 months, and 10 months of pregnancy.
At the end
When ultrasound is placed from the side to the fetal head, acoustic shadow occurs below the skull base and the top of the head as shown in Fig. 1, but in the central part of the baby's head, ultrasonic attenuation is less, and acoustically it plays the role of "window", and reading below it becomes rather easy. In this way, the fetal head assists in UOC measurement and does not interfere with it.
To measure the UOC, it is necessary to descend into the pelvis of the fetal head, which has developed to a certain size. UOC can be measured from around 28 weeks of pregnancy. In the case of the breech presentation, it becomes difficult to measure.
If you get used to this method, it will be possible to examine each pregnant woman health checkup and even during the delivery process as if you are taking X-rays many times with the Guthmann method.
According to the definition of the Terminology Committee of the Japanese Society of Obstetrics and Gynecology, OC (obstetric conjugate) is less than 9.5 cm narrow pelvis, and 9.5 to 10.4 cm is relatively narrow pelvis. Dr. Hiromitsu Yamazaki pointed out the following in Reference 2) about this reference value.
"These reference values are set very severely, and for example, "elementary school girls are prone to difficulties because they are narrow pelvises". Even if what they are saying is correct, there are few things that are actually useful because elementary school students do not give birth. I agree so too. I think this definition should be changed to what was in modern women. Personally, I would like the OC to be defined as a narrow pelvis of less than 10 cm and a relatively narrow pelvis of less than 10 to 11 cm. I think that the average value of OC is about 12cm is reasonable.
I say Again, UOC is deferent from OC. In my research, the minimum value of UOC was 10.9 cm and the average value was about 13 cm. UOC seems to be measured about 1cm longer than OC. From my experience, according to ultrasound diagnosis, I would like to advocate that less than UOC 11cm is narrow pelvis and less than UOC11-12cm is relatively narrow pelvis.
At present, less than 80 degrees is abnormal for pelvic opening angle measurement by ultrasound.
There will be many objections. It would certainly be impossible to diagnose CPD by ultrasound. "Don't say anything ambiguous. It seems to be said. However, we want to reduce even one case of severe neonatal asphyxia and cerebral palsy.
Another theme is the diagnosis of sacral morphological abnormalities caused by ultrasonic tomography. As shown in Fig. 16, if UOC is measured in UOC ①, UOC ②, and UOC ③, we think that sacral morphological abnormalities can be diagnosed to some extent. Currently, we are investigating three types: Ⓐ flat type, Ⓑ double promontory, and Ⓒ funnel type. (Fig-17)
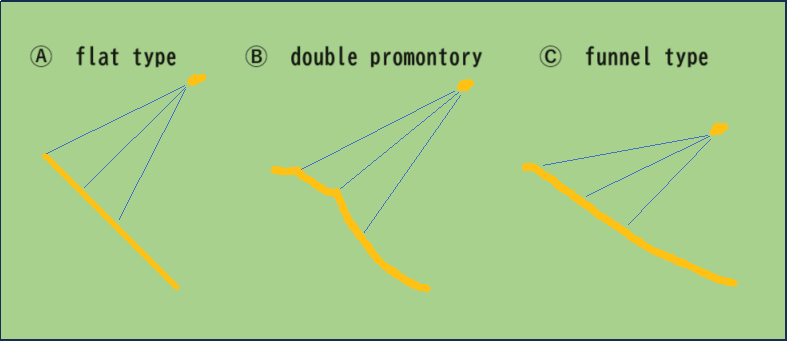 Figure-17
Figure-17Reference 1)
Katanosaka M, Yoshinaga M, Fuchiwaki K, Nagata Y.
Measurement of obstetric conjugate by ultrasonic tomography and its significance. Am J Obstet
Gynecol,1999;180:159-162
Reference 2)
Mathematical Analysis of CPD Determination Hiromitsu Yamazaki, ペリネイタルケア1994;13(3):204-216
〒885-0085
宮崎県都城市平塚町3016
TEL:(0986) 22-4585 FAX:(0986) 22-3925
外来診療日
| 月 | 火 | 水 | 木 | 金 | 土 | 日/祭 | |
|---|---|---|---|---|---|---|---|
| 午前 | |||||||
| 午後 |
午前:9:00~12:30 / 午後:14:00~17:30
休日・時間外・夜間の電話応対・診療はできません。
